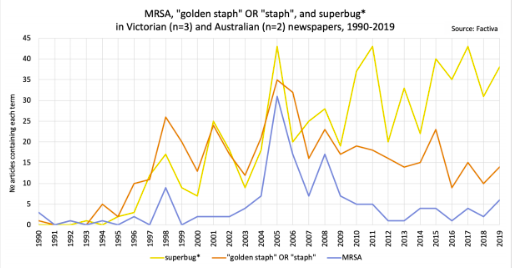
News media interest 1990-2019 (source: Davis et al., 2020b).
Context
This case study comes from AMR: Science, Communications and Public Engagements (AMR-scapes), based at Monash University in Melbourne, Australia. Global and national policy frameworks make reference to the need to involve members of the general public in efforts to reduce antimicrobial resistance, including close adherence to prescription guidelines for antibiotics. In addition, individuals in Australia can access antibiotics on prescription and funded by the government at low cost (Pharmaceutical Benefits Scheme, PBS), making antibiotic consumption highly regulated. Government data shows that use of antibiotics has somewhat declined since 2016 and 2017, the first drop since the 1990s (ACSQHC, 2019). In 2017, 41.5% of the population was dispensed an antibiotic under the PBS (ACSQHC, 2019).
In 2019, Australia launched its second national strategy which focusses on ‘whole of society’ awareness and action, among other approaches (Australian Government, 2020). We analysed Australian news media and health communications on AMR alongside in-depth interviews with 99 socially diverse individuals in Melbourne about their experiences of using antibiotics and how they explained the concept of antimicrobial resistance. The research aimed to generate a new qualitative database to help inform Australian policy and communications on AMR (Davis et al., 2021).
Promoting public awareness and action on AMR through policy and communications
Public understanding
Research, including that of AMR-scapes, shows that most individuals do not understand how they could contribute to the prevention of AMR, partly because they understand the management of infections in terms of immunity as bodily self-defence (Lohm et al., 2020; Davis et al., 2020a; Norris et al., 2013; Brooker-Howell et al., 2012). For this reason, individuals often say that their bodies become resistant to antibiotics. In addition, healthcare is often seen as an individual life project or a parental or carer’s responsibility (McNay, 2009). These understandings can interfere with messaging on the reduction of AMR which seeks collective effort to protect the healthcare of future generations.
Communications and news media
In Australia since 2000, public health campaigns have attempted to correct mistaken beliefs and establish norms for compliant use, with limited impact (Price et al., 2018). International evidence shows that social media (Antibiotic Guardian; Twitter) used to prevent AMR tend to reach individuals employed in health care and AMR fields but not so much the rest of the general public (Newitt et al., 2019; Cumbraos-Sánchez et al., 2019). Less well understood is how AMR messaging could be integrated into online health information services, emerging online script services, and related digital health care products (Brown and Netleton, 2017).
AMR-scapes analyses of news media show that AMR is mostly depicted as a niche, science story, featuring the heroic efforts of scientists and medical professionals, and less often the tragic stories of superbug victims (Davis et al., 2020b). News media rarely depict the action that individuals can take to prevent AMR. This is problematic since it conveys the impression that science will solve AMR and that therefore there is little individuals need do (Davis et al. 2020b).
Using antibiotics
Research often depicts members of the general public as misusing antibiotics and demanding them when they are not needed, in ways that have been attributed to their lack of understanding of microbiology (Pan et al., 2016). AMR-scapes found that individuals spoke of themselves as compliant with medical expertise, and made reference to medical practitioners who were too willing to prescribe antibiotics (Davis et al., 2020a). This polarised system of AMR blame – doctors blame patients; patients blame doctors – indicates that antibiotic use is loaded with moral judgement and norms of good health citizenship. AMR messaging that confers responsibility on publics, or medical professionals, is likely to further feed this polarised blame game and alienate audiences.
AMR-scapes also showed that antibiotic use arises in response to infections in ways that depend on material and symbolic settings, including responding to the health needs of a pet; prophylactic use of antibiotics due to travel; caring for a child with an infection; early intervention for those with recurrent infections; and selfcare prior to consulting a medical practitioner. AMR-scapes data show that antibiotics have meanings beyond their impact on microbial pathogens. For individuals, these social properties of antibiotics solve the pressing practical challenges of life and social norms of selfcare. These practices reflect longstanding marketing of health care products as solutions and particularly the reputation of antibiotics as highly effective. The practical, situatedness of antibiotic use and its social properties may provide opportunities for tailored and targeted support for the promotion of appropriate antibiotic use decision-making.
Our analyses also pointed to a schism between general publics and AMR experts. AMR is distinctive compared to other health problems because it lacks a ‘community of interest’, for example, cancer survivors, people with COPD, or people with HIV. AMR is also difficult to comprehend without some basic microbiological knowledge, as research has shown. The dominance of scientific discovery narrative on AMR in news media underlines this schism between lay and expert publics. A key challenge for AMR communications pertains to effective dialogue between lay and expert publics to fashion new alliances, messages and narratives for the prevention of AMR.
Conclusion
Helping members of the general public endorse and assist with the careful and moderated use of antimicrobials will depend on close attention to the meanings loaded onto these pharmaceuticals and the social contexts and biographical circumstances within which they are sought out and consumed.
Points of discussion
Pedagogical notes
For new students:
For advanced students:
Community Engagement and Policy Lead, Centre to Impact AMR and Associate Professor, School of Social Sciences, Monash University.